
The high rate of diseases in Indonesia shows that there is room for improvements Indonesian health system. A health system is built by six main aspects, including good health services, well-performing health workforce, well-functioning health information system, good health financing system, as well as leadership and governance.1 One of the main issues that we focus on is a good health financing system. These are seen through the effect of the roughly distributed implementation of the national health system (Sistem Kesehatan Nasional, abbreviated as SKN), low financing (2.2% of Gross Domestic Product while the standard recommended by WHO is 5%), and the unbalanced ratio of health workers to the population.2
In order to improve health outcomes in Indonesia, constant improvements of the national health system is needed. To do so, we can learn from experiences of other countries. By obtaining information about different health systems, a critical attitude and motivation will emerge from the community to improve SKN and increase the welfare of the people.
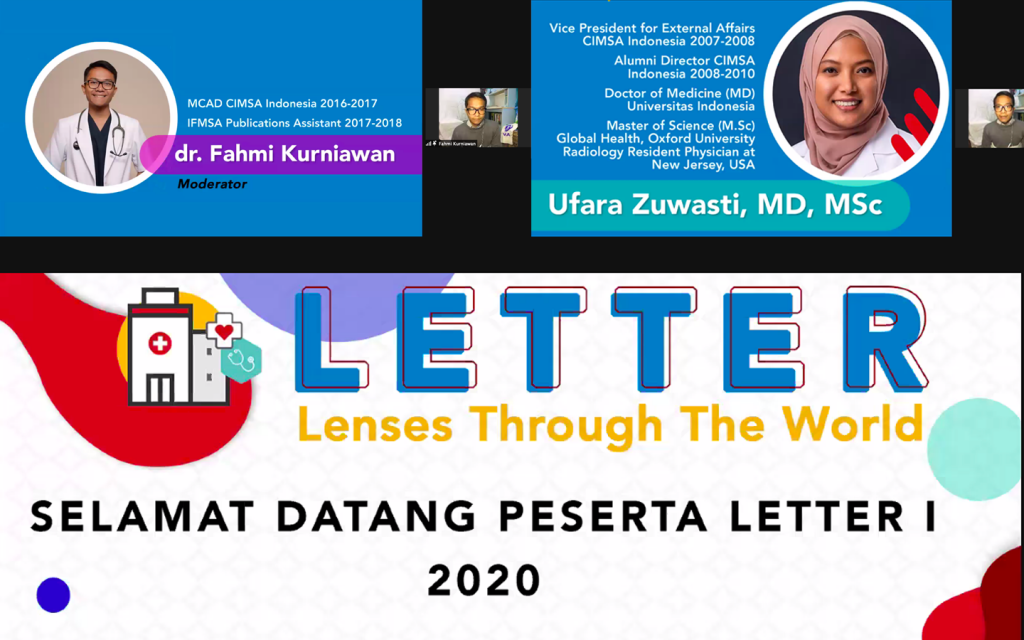
Through one of our Local Committees Event, Lenses Through The World (LETTER), many questioned the reason why the health aspect is greatly associated with health system financing. In certain places, it is an undeniable fact that healthcare is a part of business3, regarding knowledge discrepancy between health providers and patients. Health providers (sellers) and patients (buyers) do not have the same knowledge unlike the economy we are more familiar with. This discrepancy enables health practitioners to increase or decrease demand depending on the health financing system, which influences a country to shape its health system.4
Another issue in the health system financing is ‘adverse selection’, where it determines how insurance works by looking at factors, such as lifestyle, age, gender, or illness. Individuals with higher risk tend to use insurance because their average premium is smaller than their risk, and vice versa. However, it may cause moral hazards to arise. Moral hazard is likened to an over-use of services because the insurer, either public or private, will pay and thus the consumer does not face the full cost. As a result, someone whose health insurance is paid no longer takes care of their own health. Thus, to reduce this moral hazard, a health regulation is made where most of the insurance we received are paid by the government in accordance to Universal Health Coverage (UHC). For example, the patients are charged with some percentage of the health cost.

Indonesian national health insurance is managed by BPJS-Kesehatan, a national insurance body. Only in 2 years, 2014 to 2016, BPJS was able to cover 171 million people and this number continues to grow. As a comparison, countries such as South Korea and Japan have reached UHC within 26 years and 36 years respectively. It means our nation’s health insurance is in demand by society.5
In Indonesia, the insurance’s revenue is done by collecting mandatory insurance premiums from individuals. There are three premium levels and each can choose which level suits them the most. BPJS payment divides the participants into two major categories, Penerima Bantuan Iuran (PBI)and Peserta Bukan Penerima Bantuan Iuran (Non-PBI),with several derivative subclasses depending on their status of occupation and family relative.6To overcome a large number of participants, BPJS and JKN-KIS must control the ratio of non-specialist case visits by optimizing health facilities from primary to advanced health care.
Beside the BPJS-Kesehatan insurance which applies nationally, there are examples of additional health financing systems in some Indonesian cities. In Central Sulawesi, if a patient does not have BPJS insurance, their health expenses will be paid by the local government as long as the patient has a regional identity card or a family card. However, this only applies in that specific area, hence the health expenses won’t be covered if the patient is referred to another area. Each local government has its own regulations regarding its health system.4

In America, health insurance called ObamaCare has similar goals and concepts with BPJS for UHC. The main difference is that ObamaCare patients pay their own fees or are funded by private parties, but patients with low stages of homelessness can also get treatment. Whereas in Costa Rica, insurance does not discriminate against people and there is also a limit for someone to pay. A situation where healthcare spending will increase as the health problems are increasing can happen, but there are ways to avoid deficits caused by this problem. Singapore has a national health insurance system called MediSave, an account for people to save part of their income for future health needs. The amount they give will be tax-free; the more they save, the more the tax is reduced.4
In conclusion, the health system will vary from country to country. We cannot compare directly and implement it as it is built by several factors; from the population, health resources, and politics. Unlike the general economic system where both parties understand what they’ve spent and expected, in health economics, only the health authorities understand the health system itself. With so, there are some imbalance dominions here. It is necessary for society to get more acknowledgement about health system finance to really understand what expectation they’ll get in order to improve the nation’s health system program.
References:
- World Health Organization. Everybody’s business: strengthening health systems to improve health outcomes [Internet]. Geneva: WHO. 2007. [cited 2020 Aug 1]. Avaiable from: www.who.int/healthsystems/strategy/everybodys_business.pdf?ua=1
- Adisasmito W. Sistem kesehatan nasional [internet]. Indonesia: Fakultas Kesehatan Masyarakat Universitas Indonesia; date unknown [cited 2020 Aug 1]. Available from: https://staff.blog.ui.ac.id/wiku-a/files/2009/10/sistem-kesehatan-nasional.pdf
- Ufara Z, Kurniawan F. Lenses Through the World “LETTER”: Financing in Health System. SCOPE CIMSA UI. presentation given on 2020 Sep 26
- Sawyer NT. In the U.S. “Healthcare” Is Now Strictly a Business Term. West J Emerg Med. 2018 May;19(3):494-495. doi: 10.5811/westjem.2018.1.37540. Epub 2018 Mar 13. PMID: 29760846; PMCID: PMC5942015.
- BPJS-Kesehatan. Ringkasan Eksekutif Laporan Pengelolaan Program dan Laporan Keuangan Jaminan Sosial Kesehatan. Jakarta: BPJS-Kesehatan. 2016. [cited Sep 26]. Available from: https://bpjs-kesehatan.go.id/bpjs/dmdocuments/b39df9ae7a30a5c7d4bd0f54d763b447.pdf
- BPJSD. Panduan Praktis tentang Kepesertaan dan Pelayanan Kesehatan yang diselenggarakan oleh BPJS Kesehatan berdasarkan Regulasi yang Sudah Terbit. [internet]. Jakarta. unknown date. [cited 2020 Nov 30]. Avaiable from https://bpjs-kesehatan.go.id/bpjs/dmdocuments/a9c04aa825ffc12d24aeee668747f284.pdf



